Targeted therapy is a type of cancer treatment that uses drugs designed to “target” cancer cells without affecting normal cells. This treatment can influence the tissue environment where cancer cells develop or target cells directly involved in cancer growth, such as blood vessel cells.
It’s effective for various types of cancer and can be combined with other treatments like chemotherapy. Compared to chemotherapy, which succeeds around 30% of the time, targeted therapy achieves up to 80% success rates. While not all cancers have targeted therapies, ongoing research expands the range of available treatments.
This article will help you understand how targeted therapy works to treat cancer.
What is Targeted Therapy?
Targeted therapy is a type of cancer treatment that targets proteins that control how cancer cells grow, divide, and spread. It is the foundation of precision medicine. As researchers learn more about the DNA changes and proteins that drive cancer, they can better design treatments that target these proteins.
Dr. Sumant Gupta, a renowned Medical Oncologist, specializes in targeted therapy for cancer. With extensive experience in this field, Dr. Gupta has helped numerous patients benefit from precision treatments that target specific genes and proteins in cancer cells. His expertise and dedication make him a trusted expert in delivering effective targeted therapy, improving outcomes for cancer patients.
What Are The Types Of Targeted Therapy?
The table below outlines the types of targeted therapy used in cancer treatment:
| Type of Targeted Therapy | Description |
| Monoclonal Antibodies | Antibodies are designed to target specific proteins in cancer cells, tagging them for destruction by the immune system. |
| Tyrosine Kinase Inhibitors | Drugs that block signals needed for cancer cell growth are often used for cancers with specific genetic mutations. |
| Hormone Therapies | Drugs that interfere with hormone production or activity are commonly used for hormone-sensitive cancers like breast or prostate cancer. |
| Angiogenesis Inhibitors | Drugs that block the formation of new blood vessels cut off the blood supply to tumors and slow their growth. |
| PARP Inhibitors | Drugs that inhibit PARP enzymes prevent cancer cells from repairing their DNA and leading to cell death. |
These therapies are often used in combination with other cancer treatments, such as chemotherapy or radiation therapy, to improve outcomes and reduce side effects.
Dr. Sumant Gupta: “Targeted therapies are personalized based on the unique characteristics of a patient’s cancer. This includes factors like specific genetic mutations or proteins in the cancer cells. By identifying these traits, we can match patients with treatments most likely effective for their particular type of cancer, maximizing the benefits of targeted therapy.”
How Does Targeted Therapy Work Against Cancer?
The following explains the different ways that targeted therapy treats cancer.
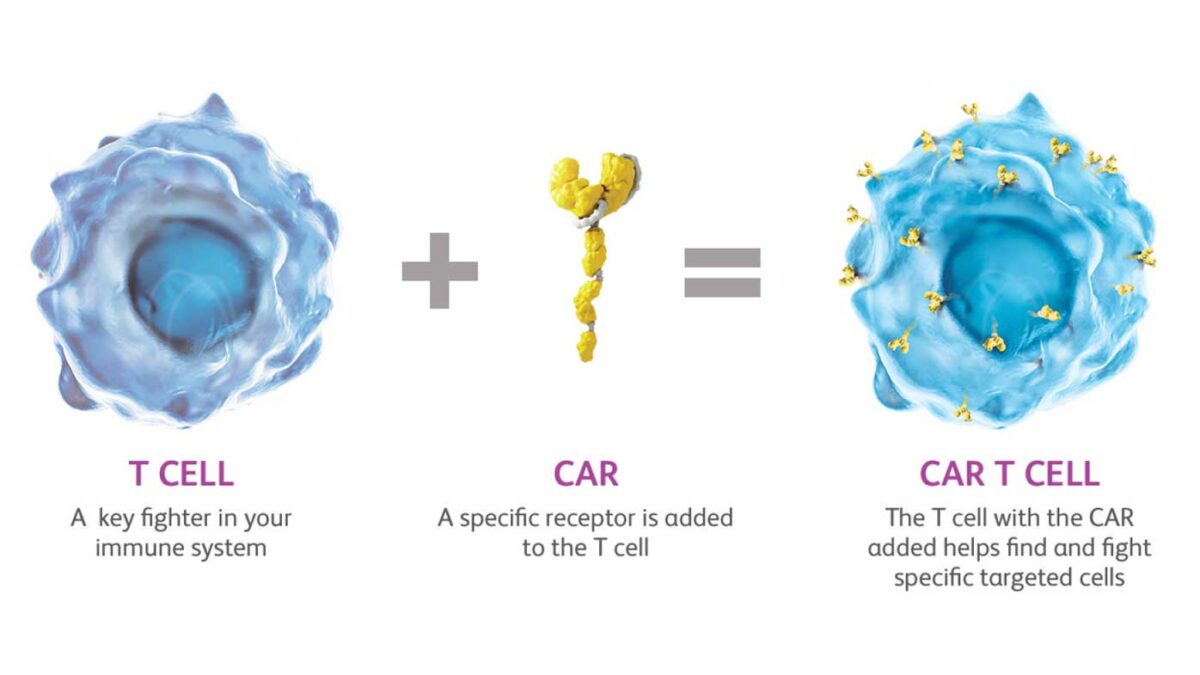
- Help the immune system destroy cancer cells: Cancer cells thrive because they can hide from your immune system. Specific targeted therapies can mark cancer cells, making it easier for the immune system to find and destroy them. Other targeted therapies help boost your immune system to work better against cancer. Learn more about immunotherapy to treat cancer.
- Stop cancer cells from growing by interrupting signals that cause them to expand and divide: Healthy cells in your body usually divide to make new cells only when they receive strong signals. These signals bind to proteins on the cell surface, telling the cells to divide. This process helps new cells form only as your body needs them. However, some cancer cells have changes in the proteins on their surface that tell them to divide whether or not signals are present. Some targeted therapies interfere with these proteins, preventing them from telling the cells to divide. This process helps slow cancer’s uncontrolled growth.
- Stop signals that help form blood vessels: To grow beyond a specific size, tumors must form new blood vessels in an angiogenesis process. The tumor sends signals that start angiogenesis. Some targeted therapies called angiogenesis inhibitors interfere with these signals to prevent a blood supply from forming. Without a blood supply, tumors stay small. Or, if a tumor already has a blood supply, these treatments can cause blood vessels to die, which causes the cancer to shrink. Learn more about angiogenesis inhibitors.
- Deliver cell-killing substances to cancer cells: Some monoclonal antibodies are combined with cell-killing substances such as toxins, chemotherapy drugs, or radiation. Once these monoclonal antibodies attach to targets on the surface of cancer cells, the cells take up the cell-killing substances, causing them to die. Cells that don’t have the target will not be harmed.
- Cause cancer cell death: Healthy cells die in an orderly manner when they become damaged or are no longer needed. But cancer cells have ways of avoiding this dying process. Some targeted therapies can cause cancer cells to go through this cell death process called apoptosis.
- Starve cancer of hormones it needs to grow: Some breast and prostate cancers require certain hormones to grow. Hormone therapies are a type of targeted therapy that can work in two ways. Some hormone therapies prevent your body from making specific hormones. Others stop the hormones from acting on your cells, including cancer cells. Learn more about hormone therapy for prostate cancer and hormone therapy for breast cancer.
“Unlike traditional chemotherapy, targeted therapy is more precise, targeting specific aspects of cancer cells. It can impact the tissue environment by inhibiting factors that promote cancer growth.” – says Dr Gupta.
“I was skeptical about targeted therapy at first, but Dr. Sumant Gupta explained everything so clearly and made me feel confident in my treatment plan. The personalized approach made a difference, and I’m grateful for the positive outcome.” – a satisfied patient of Dr. Gupta.
“I had been struggling with side effects from chemotherapy, but targeted therapy offered a more precise and effective option. Dr. Gupta’s expertise and the tailored treatment plan have significantly improved my quality of life. I highly recommend considering targeted therapy for cancer treatment.” – another pleased patient.
How Much Does Cancer Targeted Therapy Cost In India?
| Targeted Therapy | Cost in INR | Cost in USD (Approx.) |
| Trastuzumab (Herceptin) | ₹75,000 – ₹1,00,000 per vial | $1,000 – $1,350 per vial |
| Bevacizumab (Avastin) | ₹25,000 – ₹35,000 per vial | $335 – $470 per vial |
| Rituximab | ₹15,000 – ₹25,000 per vial | $200 – $335 per vial |
| Imatinib (Gleevec) | ₹8,000 – ₹10,000 per month | $110 – $135 per month |
Please note that these costs are approximate and vary based on the dosage, brand, and hospital or clinic. It’s advisable to consult with a healthcare provider or pharmacist for the most accurate and up-to-date pricing information.
Conclusion
Targeted therapy is like using a smart missile to attack cancer cells, leaving healthy cells unharmed. It’s a precise approach that has improved outcomes for many patients. While it’s not a cure-all, and some challenges remain, like the risk of resistance, it’s a significant step forward in cancer treatment. As research continues, we can expect even more progress in fighting cancer with targeted therapy, giving hope to those battling this disease.
FAQs about Targeted Therapy
-
Can targeted therapy be used alone to treat cancer?
Targeted therapy is often used in combination with other treatments like chemotherapy or radiation therapy to improve outcomes.
-
Are there side effects of targeted therapy?
Yes, common side effects include diarrhea, skin problems, and high blood pressure, but they can vary depending on the specific therapy.
-
Is targeted therapy a one-size-fits-all approach?
No, targeted therapy is tailored to the specific genetic makeup of an individual’s cancer cells.
-
How is targeted therapy different from traditional chemotherapy?
Targeted therapy specifically targets cancer cells, while chemotherapy affects all rapidly dividing cells, including healthy ones.
-
Can targeted therapy fully cure cancer?
While targeted therapy can be highly effective, it’s not always a cure. It can help control cancer and improve quality of life.
Read More : What Are The Various Cancer Screening Options?
Globally, cancer remains a significant health concern, with millions of new cases diagnosed each year. Cancer screening emerges as a pivotal tool in the quest for early detection. These tests are designed to detect signs of cancer before symptoms manifest, offering a crucial window for intervention.
In the ever-evolving landscape of cancer, solid tumors continue to impact lives globally. According to recent statistics, solid tumors accounted for approximately 75% percentage of cancer diagnoses in 2023, highlighting their prevalence and significance on a global scale.
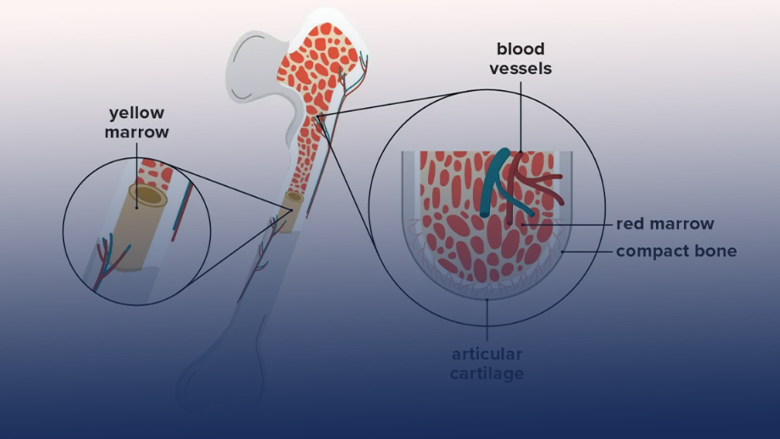
In today’s medical landscape, bone marrow transplants (BMTs) have emerged as powerful treatments, offering hope to individuals battling severe health conditions. About 50,000 people worldwide undergo these transformative procedures each year, aiding those afflicted with cancers, blood disorders, and immune deficiencies. These transplants work like a cellular rescue mission, replacing damaged or diseased bone marrow with healthy stem cells, bolstering the body’s ability to produce essential blood cells.
BMT success varies based on the type used. This blog delves into the success rates of bone marrow transplants, shedding light on their impact on patients’ lives. It explores the advancements driving their success, unraveling the complexities behind these transformative procedures.
What Is A Bone Marrow Transplantation?
A bone marrow transplant (BMT) involves infusing healthy stem cells into a patient’s bloodstream to replace damaged or diseased bone marrow. This procedure treats certain cancers, blood disorders, or immune system deficiencies by replenishing healthy cells capable of producing blood cells. BMT may use cells from the patient (autologous), a matched donor (allogeneic), or umbilical cord blood.
The primary objective of a bone marrow transplant is to repopulate the bone marrow with healthy stem cells. This process restores the marrow’s capacity to produce healthy blood cells, offering a potential cure or better management for life-threatening conditions.
Dr. Sumant Gupta performed the first-ever Bone Marrow Transplant in Faridabad. His pioneering work brought a new ray of hope to patients facing serious health challenges. His work has offered vital treatment options and paved the way for further progress in healthcare.
What Factors Influence the Success Rates Of BMT?
Several factors significantly influence bone marrow transplant (BMT) success:
- Patient’s Health: Overall health determines the body’s ability to endure the transplant process and recover post-surgery.
- Cell Source: Autologous transplants boast higher success rates as they use the patient’s cells, reducing rejection risks.
- Donor Match: Allogeneic transplants require well-matched donors for better outcomes; a close match minimizes the risks of complications.
- Underlying Diseases: The type and severity of the underlying condition affect transplant success and post-transplant recovery.
- Pre-Transplant Preparations: Adequate pre-transplant assessments and preparations contribute to better outcomes, reducing risks and complications.
What Are Global BMT Success Rates?
Global success rates for bone marrow transplants vary based on transplant types:
- Autologous Transplants: Autologous transplants have high success rates, over 90%. This happens because these transplants use the patient’s cells, reducing the chances that the body will reject them. This personalized approach increases the likelihood of the transplant’s success, offering a better opportunity for treatment and recovery.
- Allogeneic Transplants: Allogeneic transplants have varying success rates, typically between 40% to 80%. The success depends on finding a suitable donor whose cells match the patient’s. When the donor’s cells are a good match, there’s a higher chance of the transplant working well. However, finding the right match can be challenging, influencing the treatment’s success.
- Matched Sibling Donor: Having a matched sibling as a donor significantly improves the chances of a successful bone marrow transplant. It increases the likelihood of living longer after the procedure, with about 70-80% of people surviving beyond a year after the transplant. This match provides a better chance for the body to accept the new cells, aiding recovery.
- Matched Unrelated Donor: When the bone marrow donor is not a sibling but someone unrelated, the chances of survival after a transplant become a bit lower. About 50-60% of people typically survive a year after this type of transplant. It’s more challenging because the body might not accept the new cells as easily, affecting the overall recovery and longevity.
“Over the last decade, advancements in technology and better understanding of immunology have positively impacted success rates and life expectancy across all transplants. Despite variations, improvements in medical advancements and donor matching techniques have notably enhanced survival rates and life expectancies, enhancing the prospects for patients undergoing bone marrow transplants globally,” mentions Dr. Sumant.
A happy and recovered patient of Dr. Sumant shared, “Having undergone a bone marrow transplant was a turning point in my life. Dr. Sumant Gupta’s expertise and the seamless procedure played a significant role in my recovery. His team’s dedication and care made the entire process smoother. Today, I’m leading a healthier life, grateful for this second chance that the transplant offered me.”
Another patient expressed, “The decision to undergo a bone marrow transplant was daunting, but Dr. Sumant and his team’s support made it manageable. Their guidance and care during and after the transplant were exceptional. I’m thankful for their expertise, which treated my condition and gave me a renewed hope for a healthier future.”
How Much Does a Bone Marrow Transplant Cost in India?
The cost of bone marrow transplants in India typically ranges from 12 to 15 lakhs for allogeneic and 8 to 10 lakhs for autologous transplants. When converted, these amounts translate to roughly $16,000 to $20,000 and $10,000 to $13,000 in USD, respectively.
These costs can fluctuate based on several factors, including the hospital’s infrastructure, medical professionals’ expertise, the possibility of complications, and the specific facilities required for the transplant process. Overall, the expenses are influenced by various elements inherent in the transplantation procedure and post-operative care.
Conclusion
Bone marrow transplants (BMTs) offer hope for treating life-threatening conditions by replenishing healthy cells. With advancements in technology and improved donor matching, BMTs have seen enhanced success rates, particularly autologous transplants, and better life expectancies for patients worldwide.
FAQs:
-
Can anyone be a bone marrow donor?
Only some people are eligible due to health factors; potential donors undergo thorough assessments.
-
How long does it take to find a donor?
Depending on donor availability, finding a suitable match can take weeks to months.
-
Are there risks associated with BMT?
Yes, risks include infection, graft-versus-host disease, and organ damage.
-
What is the typical recovery time post-BMT?
Recovery may take several months to a year or more for complete recovery.
-
Can BMT cure all diseases?
No, BMT is effective for specific cancers, blood disorders, and immune deficiencies.
Read More : What Are The Warning Signs of Head and Neck Cancer?
Copyright by www.drsumantgupta.com. All rights reserved.